📌 Table of Contents
- Introduction
- What is Type 2 Diabetes?
- Global Prevalence and Statistics
- Causes and Risk Factors
- How Type 2 Diabetes Develops
- Symptoms and Early Warning Signs
- Diagnosis and Testing
- Health Complications from Type 2 Diabetes
- Treatment Options
- Lifestyle Management
- Diet and Nutrition
- Physical Activity and Exercise
- Medications and Insulin Therapy
- Monitoring Blood Sugar Levels
- Mental Health and Diabetes
- Diabetes in Children and Adolescents
- Diabetes and Pregnancy
- Technology in Diabetes Management
- Living with Type 2 Diabetes
- Prevention Strategies
- Community and Support Systems
- The Economic Burden of Type 2 Diabetes
- Future of Diabetes Treatment
- Conclusion: A Call to Action
Introduction
Type 2 Diabetes Mellitus (T2DM) has quietly evolved into one of the most significant global public health challenges of the 21st century. While largely preventable, its increasing prevalence reflects the modern lifestyle — sedentary behavior, poor dietary habits, and widespread stress. This blog post explores every angle of this chronic condition, with the aim of offering insight, knowledge, and hope.
What is Type 2 Diabetes?
Type 2 diabetes is a metabolic disorder characterized by insulin resistance and relative insulin deficiency, leading to elevated blood glucose levels. Unlike type 1 diabetes, which is an autoimmune condition, type 2 develops over time and is largely linked to lifestyle and genetic factors.
Global Prevalence and Statistics
- According to the *International Diabetes Federation, over *537 million adults lived with diabetes in 2021.
- 90–95% of those diagnosed with diabetes have Type 2.
- Projections estimate over 783 million people will have diabetes by 2045.
- Countries like India, China, and the U.S. face a diabetes crisis due to urbanization and lifestyle shifts.
Causes and Risk Factors
1. Genetics
- Family history increases the likelihood.
- Certain ethnic groups (Africans, Latinos, South Asians) are at higher risk.
2. Obesity
- Visceral fat (belly fat) promotes insulin resistance.
- BMI ≥ 30 significantly raises the risk.
3. Physical Inactivity
- Sedentary lifestyle contributes to insulin resistance.
4. Poor Diet
- High intake of sugar, refined carbs, and saturated fats.
- Low intake of fiber and whole grains.
5. Age
- Risk increases after age 45.
6. Other Conditions
- Hypertension, high cholesterol, and PCOS are linked.
How Type 2 Diabetes Develops
Stage 1: Insulin Resistance
The body’s cells become less responsive to insulin, requiring more insulin to maintain normal glucose levels.
Stage 2: Hyperinsulinemia
The pancreas compensates by producing more insulin, leading to higher insulin levels in the blood.
Stage 3: Beta-Cell Dysfunction
Over time, pancreatic beta cells deteriorate, reducing insulin production.
Stage 4: Hyperglycemia
With insufficient insulin, glucose builds up in the bloodstream, resulting in type 2 diabetes.
Symptoms and Early Warning Signs
- Increased thirst and urination
- Fatigue
- Blurred vision
- Slow-healing wounds
- Frequent infections
- Tingling or numbness in hands and feet
- Darkened skin in certain areas (acanthosis nigricans)
Diagnosis and Testing
1. Fasting Blood Glucose Test
- Normal: <100 mg/dL
- Prediabetes: 100–125 mg/dL
- Diabetes: ≥126 mg/dL
2. Oral Glucose Tolerance Test (OGTT)
3. HbA1c Test
- Reflects average blood glucose over 3 months
- Diabetes: ≥6.5%
4. Random Blood Sugar Test
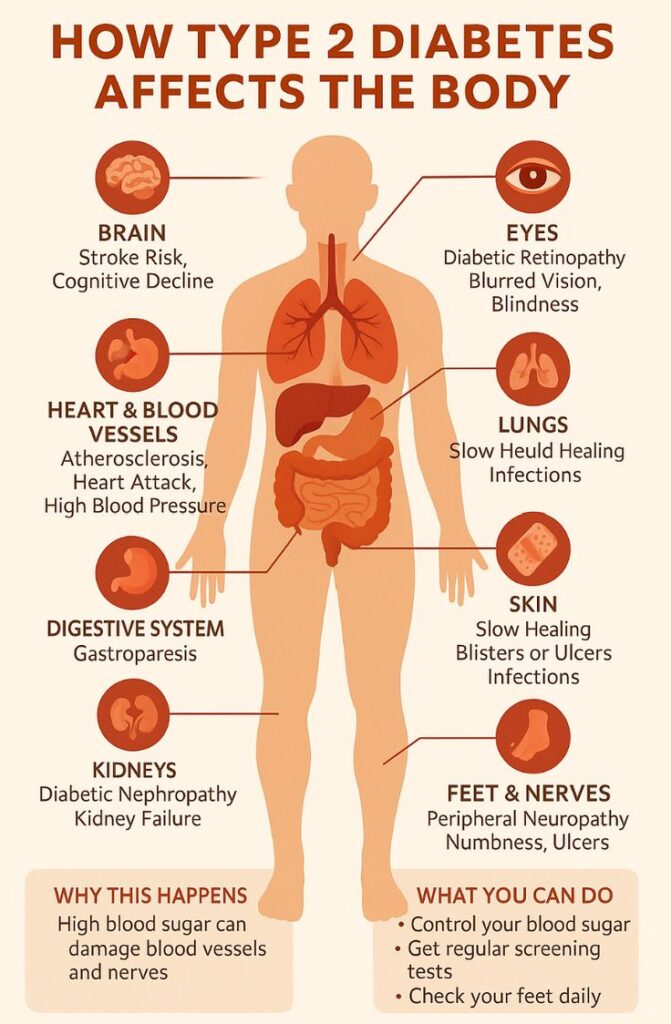
Health Complications from Type 2 Diabetes
Short-term
- Hypoglycemia (low blood sugar)
- Hyperosmolar Hyperglycemic State (HHS)
Long-term
- Cardiovascular Disease
- Kidney Disease (Nephropathy)
- Eye Disease (Retinopathy)
- Nerve Damage (Neuropathy)
- Foot Ulcers and Amputation
- Cognitive Decline/Dementia
Treatment Options
1. Lifestyle Intervention
- Diet and exercise are first-line therapies.
2. Oral Medications
- Metformin
- Sulfonylureas
- DPP-4 inhibitors
- SGLT2 inhibitors
- GLP-1 receptor agonists
3. Insulin Therapy
- Basal and bolus regimens in advanced cases.
Lifestyle Management
Lifestyle changes remain the cornerstone of management:
- Reducing body weight by even 5–10% can improve outcomes.
- Daily tracking of blood sugar, activity, and meals helps identify patterns.
Diet and Nutrition
Best Foods for Type 2 Diabetes:
- Whole grains (quinoa, brown rice)
- Leafy greens
- Nuts and seeds
- Lean proteins (chicken, fish)
- Legumes and beans
Foods to Avoid:
- Sugary drinks
- Processed snacks
- White bread and rice
- Fried foods
Portion Control and Carb Counting:
- Carb management is essential in maintaining glucose levels.
- Use of apps and dieticians can help with meal planning.
Physical Activity and Exercise
- 150 minutes/week of moderate aerobic exercise recommended.
- Resistance training twice a week improves insulin sensitivity.
- Even walking after meals can reduce blood sugar spikes.
Medications and Insulin Therapy
Oral Medications
- Metformin: First-line medication, reduces liver glucose output.
- SGLT2 inhibitors: Help excrete glucose via urine.
- GLP-1 receptor agonists: Promote satiety and weight loss.
Insulin Types
- Rapid-acting
- Long-acting (Basal)
- Premixed insulin
Monitoring Blood Sugar Levels
Why Monitor?
- Helps prevent highs and lows.
- Informs medication adjustments.
Tools
- Glucometers
- Continuous Glucose Monitors (CGMs)
Mental Health and Diabetes
- Depression and anxiety are common comorbidities.
- Support groups and therapy can help manage the emotional toll.
Diabetes in Children and Adolescents
Type 2 diabetes in youth is rising due to:
- Childhood obesity
- Inactivity
- Unhealthy diet
Early diagnosis and aggressive lifestyle changes are essential.
Diabetes and Pregnancy
Gestational diabetes can progress to Type 2 later. Managing glucose during pregnancy is critical to avoid:
- Birth complications
- Preeclampsia
- Childhood obesity in the baby
Technology in Diabetes Management
- Smart Insulin Pens
- CGMs like Dexcom and FreeStyle Libre
- Mobile Apps for tracking meals and medications
- AI-driven platforms for personalized plans
Living with Type 2 Diabetes
Success stories show that many people reverse or manage diabetes through:
- Weight loss
- Intermittent fasting
- Vegan or low-carb diets
- Dedicated exercise routines
Prevention Strategies
1. Public Health Campaigns
- Promoting awareness about symptoms and risk factors.
2. Education Programs
- Schools and workplaces should educate on healthy lifestyle habits.
3. Screening and Early Detection
- For high-risk populations, annual testing can catch prediabetes early.
Community and Support Systems
- Family support improves treatment adherence.
- Online communities offer emotional connection.
- Support groups reduce stress and promote accountability.
The Economic Burden of Type 2 Diabetes
- Costs global economies over \$966 billion annually.
- Indirect costs: lost productivity, disability, premature death.
- Reducing incidence can save billions in healthcare costs.
Future of Diabetes Treatment
Emerging Research Areas:
- Beta-cell regeneration
- Gut microbiome therapy
- Gene editing (CRISPR)
- Smart insulins that respond to glucose levels
- Artificial pancreas systems
Conclusion: A Call to Action
Type 2 diabetes doesn’t have to be a life sentence. With education, proactive lifestyle choices, and community support, it can be prevented, controlled, or even reversed. Governments, individuals, and health institutions must act in unison to combat this global threat.
🌐 Tags:
- #Type2Diabetes
- #HealthAndWellness
- #DiabetesManagement
- #Nutrition
- #PreventiveCare
- #Fitness
- #ChronicDisease